Twin to Twin Transfusion Syndrome
Australia Inc.
What is TTTS?
Twin to Twin Transfusion Syndrome is a very complex problem affecting approximately 15% of identical twin pregnancies. Information has been grouped in the following categories:
- Types of Twins
- What is Twin to Twin Transfusion Syndrome?
- Symptoms of TTTS
- What are the treatment options?
- Medical Information Provided by Australian Hospitals
Types of TwinsBefore TTTS can be understood, it is helpful to know how twins occur and the different types that can be conceived.
Dizygotic (Fraternal) twins occur when the mother releases 2 eggs during one ovulation cycle and these are then fertilised. Fraternal twins are no more alike than any other brother or sister except that they share the same birthday. They can be the same sex or boy-girl. All dizygotic twin pregnancies have 2 choria (outer membrane) and 2 amnia (inner membranes). Most have 2 separate placentae. If the twins implant in the uterus close together, the placentae can fuse so that it appears that there is only 1. These twins would still have 2 choria and 2 amnia. (see Fig 1 and 2)
Monozygotic (Identical) twins occur when a single zygote (fertilised ovum) divides during the first two weeks of development. If the division occurs during the first 5 days, there will be 2 choria, 2 amnia and either separate or fused placentae. This occurs in approximately 33% of cases. (see Fig 1 and 2)
If the division occurs between days 5 and 10, there is one chorion (outer membrane) and two amnia (inner membranes) with one placenta. This occurs in approximately 63% of cases. (see Fig 3)
If the division occurs between day 10 and day 14, there is one placenta, one chorion and one amnion. This can be very dangerous as the babies’ cords can twist around each other possibly resulting in a diminished supply of fresh nutrients. (see Fig 4)
If the division occurs after day 14, the risk of conjoined or “Siamese” twins is extremely high.
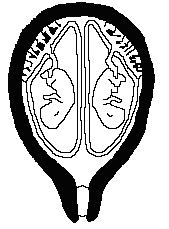
Fig 1 – This diagram shows 2 choria, 2 amnia and separate placentae.This will occur in approximately 19% of monozygotic and 58% of dizygotic pregnancies 1
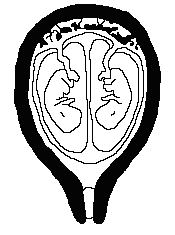
Fig 3 – This diagram shows 1 chorion, 2 amnia and a single placenta. This will occur in approximately 63% of monozygotic pregnancies 1
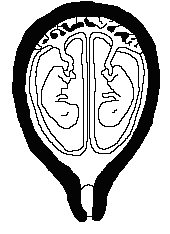
Fig 2 – This diagram shows 2 choria, 2 amnia and a fused placenta. This will occur in approximately 14% of monozygotic and 42% of dizygotic pregnancies 1
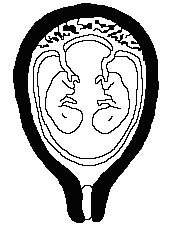
Fig 4 – This diagram shows 1 chorion, 1 amnia and a single placenta. This will occur in approximately 4% of monozygotic pregnancies 1
What is Twin to Twin Transfusion Syndrome?
Twin to Twin Transfusion Syndrome occurs in approximately 15% of monozygotic twin pregnancies. It can appear at anytime during the pregnancy and only if the pregnancy is monochorionic (ie identical twins sharing one choria and therefore, one placenta). Normally blood flows evenly between the fetuses through vessels on the placenta. (see Fig 5)
In TTTS, the blood flow is unbalanced resulting in a “donor” twin donating blood through the placenta to a “recipient” twin. (see Fig 6)
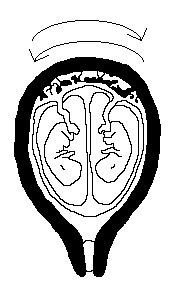
Fig 5 – This diagram shows a monochorionic pregnancy with equal blood flow between both babies 1
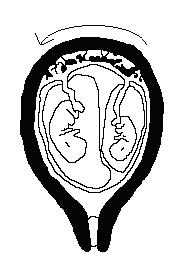
Fig 6 – This diagram shows a monochorionic pregnancy affected by TTTS. Note the smaller baby on the right with a reduced amniotic fluid level. The blood flow between the twins is uneven going from the twin on the right to the twin on the left 1
Since the donor twin is pumping blood, not only for itself but also across to the other twin, it has less energy to use in growing. This results in a smaller than average baby (sometimes noted as suffering from intrauterine growth retardation (IUGR)) with a smaller than average amniotic fluid level (oligohydramnios). When examined by ultrasound the baby’s bladder will be small or unable to be seen due to the lack of growing being done by the baby. Sometimes the baby will be almost wrapped in its amniotic membranes due to the lack of amniotic fluid. Hence the condition is occasionally referred to as stuck twin syndrome.
The recipient, however, is trying to do too much growing due to the excess blood and fluid being sent from the donor twin. This extra work results in the baby urinating more causing an abnormally large amount of amniotic fluid around them (polyhydramnios). This extra work can also cause heart failure. The recipient twin’s body cavities may accumulate fluid and can result in a condition called ‘hydrops’. If the recipient twin develops hydrops, its life is seriously threatened.
TTTS can happen at anytime during a monochorionic pregnancy. It can also occur in triplet or higher order pregnancies that include monochorionic twins.
The risks of TTTS to the twins depend on when the condition occurs. If the condition occurs late in the pregnancy, the risks are usually minimal. If one twin threatens to develop hydrops, the babies may be delivered. Of course the later in the pregnancy the delivery occurs, the safer the babies are.
One risk of TTTS is Preterm Premature Rupture of Membranes (PPROM). This is due to the increased pressure and increased amount of amniotic fluid (polyhydramnios) around the recipient twin.
The donor twin has the highest risk of dying in utero and may be born with anemia due to the lack of blood in the baby’s system. They may require a blood transfusion after birth.
The recipient twin is in danger also and may develop heart failure (hydrops) due to the excess fluid and blood. If the transfusion is chronic, the recipient’s blood may be thicker. If hydrops is present as well, the risk of a blood vessel becoming blocked is higher.
If a fetus dies in utero, the surviving twin is also at a very high risk of dying. If the baby survives there is high chance of heart or brain damage.
TTTS can be either chronic or acute. Chronic TTTS can present itself in the early months of the pregnancy meaning that the babies are too immature to be delivered when it is first detected. Acute TTTS can occur at any stage in the pregnancy, even during delivery and can cause death or disability.
TTTS is a very cruel condition. The babies are perfectly normal; the problem is with the placenta.
Symptoms of TTTS
In the Mother:
- Sudden weight gain
- Fundus appears large for dates (often will appear like a term pregnancy)
- Abdominal pain and tightness
- Premature onset of contractions
In the Babies:
(Determined by ultrasound assessment):
- Evidence of a monochorionic (shared) placenta
- Same sex twins
- Thin, hard to find, separating membrane
- One twin may be much larger than the other
- Different size bladders in each twin
- Polyhydramnios around one twin (more than 8cm pocket) and minimal amount of amniotic fluid around the other twin (less than 2cm pocket).
TTTS is diagnosed after an ultrasound is performed. Ideally, once identical twins are diagnosed, ultrasound scans should be performed at regular intervals so that if TTTS develops, treatment can begin as soon as possible.
What are the treatment options for TTTS?
The treatment options that have been used include:
Expectant management or observation
In this option, the pregnancy is monitored with ultrasound examinations. Unfortunately, expectant management is associated with pregnancy loss rate of more than 90%.
Serial amniocenteses/ Amnioreduction
This is a procedure whereby amniotic fluid is drained from the sac of the recipient twin. The aim of this treatment is to reduce the risk of preterm birth from over-distension of the uterus.
An amniocentesis needle is inserted into the sac around the recipient twin and fluid is removed until there is a normal amount around the twin. Usually 1-3 litres of amniotic fluid may be removed and this may need to be repeated every few days or weeks. Whilst there is a small procedure-related risk of rupture of the membranes and premature delivery, it does appear effective in allowing the pregnancy to continue. Unfortunately, it does not treat the underlying pathology – the transfusion of blood via the vascular connections in the placenta.
This has been the most widely used treatment in most Fetal Medicine Centres around the world. Results have shown that only about 60% of babies will survive. Of major concern is the finding that 20-25% of the survivors may have subsequent neurological complications or cerebral palsy.
Septostomy (Only offered at certain hospitals)
When the donor twin has no amniotic fluid around it, the membranes are wrapped tightly around it. Septostomy is where a needle is inserted into the uterus to deliberately make a hole in the amniotic membrane to allow fluid to get into the donor twin’s sac from the recipient twin. The aim is to try to equalise the amounts of fluid between the twins. Currently, there is little evidence to suggest that this is more effective than amnioreduction, and other complications can occur as a result of this procedure.
Umbilical cord occlusion (Only offered at certain hospitals)
If severe TTTS results in the death of one of the twins in the womb, there can be further transfusion of blood, which could cause the loss of, or severe damage to, the other twin. In severe cases of TTTS, one of the twins may become extremely sick, and can be at high risk of dying soon. If the twins are mature enough by this stage, they should be delivered. However, if this occurs before the twins are at a viable gestation, some doctors may suggest occluding the cord of the sick twin to protect the second twin from the consequences of a severe transfusion during the death of the sick twin. Cord occlusion can be done by passing an instrument into the uterus and either heat coagulating or tying off the cord of the sick twin with a suture. This interrupts the vascular communication between the twins, and allows the remaining twin to progress on its own.
Whilst this protects the second twin, it obviously causes the immediate loss of the sick twin.
Fetal laser surgery:
TTTS occurs as a result of transfusion of blood via vascular connections on the surface of the placenta. Over the past 10 years, a new treatment option has been developed. By passing a small telescope (called a fetoscope) into the uterus and identifying the connecting blood vessels on the surface of the placenta, laser surgery can be delivered by a fibre to coagulate (seal) these connections and stop the process of TTTS. This procedure has been available in a few centres overseas, and has only been available in Australia since October 2001. Whilst the overall survival rate appears to be similar to that of amnioreduction, the long term outcomes and incidence of cerebral palsy appears to be much less (about 5%) when compared with amnioreduction (15-25%). The other advantages of this procedure are that even if one of the unborn babies dies, the other twin is less likely to be harmed as there are no longer vascular communications between the babies. The main advantage of laser therapy over serial amniocentesis is that it does address the underlying cause of TTTS, and usually requires only one intervention.
The vital key to success is in meticulous selection of the vessels for coagulation to interrupt the communication between the twins. Vessels not contributing to the communication process need to be spared to maximise the chance of survival of both twins.
A video and photo images of fetal laser surgery is available by clicking here.
Medical Information Provided by Australian HospitalsThe Mater Centre for Maternal Fetal Medicine, Brisbane have kindly offered to share their information with us. Click here to connect directly to their site with information about TTTS.
Click here for a direct link to The Maternal Fetal Medicine Service of Western Australia.
The NSW Twin-Twin Transfusion Treatment Group have permitted us to publish a copy of their Patient Information. Press here to view this page.
1 Zygosity and Placentation in Twins, Prof Nick Martin, Queensland Institute of Medical Research, Australian National Health and Medical Research Council Twin Registry.